It took me a while, but I eventually noticed a pattern: It was the last of Christian’s track meets and I had just finished watching the closing races of the season. Long distance races have always intrigued me because they are lengthy enough for a narrative to develop, for a back and forth, for a test of stamina, for the dramatic come back win. But it wasn’t the dynamics of victory that caught my attention on Thursday. It was the reaction of the crowd to the various participants in the race. Predictably, the first few runners got the cheers of victory. But so did the very last runners, especially if they were way behind and struggling. We feel for the underdog, the determined “loser.” But what about those in between runners? What did they get? Wild cheers from their parents, perhaps (or sometimes suppressed disappointment). But from the crowd at large? Mild interest, half-hearted applause, if that. But mostly, they were invisible, extras to frame the exploits of the first runners and the determination of the last.
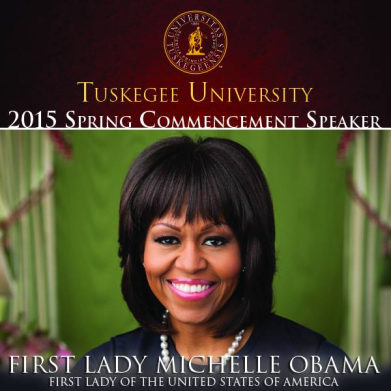
Invisibility has been on my mind since Michelle Obama mentioned the idea in her speech earlier this week at Tuskegee University. She spoke of the challenges of the African American experience this way:
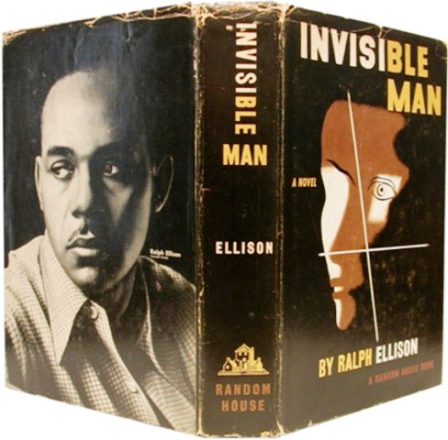
“So there will be times, just like for those Airmen, when you feel like folks look right past you, or they see just a fraction of who you really are . . . the realization that no matter how far you rise in life, how hard you work to be a good person, a good parent, a good citizen — for some folks, it will never be enough. And all of that is going to be a heavy burden to carry. It can feel isolating. It can make you feel like your life somehow doesn’t matter — that you’re like the invisible man that Tuskegee grad Ralph Ellison wrote about all those years ago.”
Some of the kids at the middle school track meet worked really hard, gave it everything and still did not end up receiving honor for their work. They were invisible.
That made me consider my own experience with invisibility.
The truth is I don’t have a harrowing story to tell. I cannot say I have felt invisible on account of my race for example . . . well, that’s not quite true. Quick context: I grew up in Kenya, biracial with a Scottish mother and a Kenyan father. In Kenya, there is a defined racial category for mixed people. We are called “point-fives”; you cannot deny the mathematical accuracy of that term! Connotation? Not derogatory at all. If anything, the term is used positively. At least, that was how I experienced the word growing up. So, like many biracial African immigrants, I came to America, and became “black” for the first time (One of my favorite comedians, Trevor Noah, has a great bit on the same experience https://www.youtube.com/watch?v=QDXWUBIUi88!). The transition to “black” took some adjustment, but was ultimately fine, except in one area, casting.
I came to America to pursue a graduate degree in Theatre (Acting) and began to notice a trend. Directors would come up to me and say “I think you’d be great for this role” and I slowly began to notice that all the roles I’d be “great for” were black roles, that is explicitly written as black characters. Many of these roles were in fact good, but in those same plays I saw many other attractive roles that were not necessarily written as black characters. I was used to being selected for roles based on the depth and layers of the character, but now part of me was invisible. To some, I was black first, an actor second (quite the adjustment after being in an all Kenyan cast of Fiddler on the Roof many years ago. Yes, you read that right; 40 Kenyans playing Russian Jews without batting an eyelid!). That said, there have been many notable exceptions: I was cast as Jack in The Importance of Being Earnest and Pooh Bah in The Mikado by directors who recognized, but did not define, my acting by my color. I respected that.
But how did the limited view that some other directors took feel? It felt restrictive of course, but perhaps also put me in touch with certain parts of the minority experience in America in a more tangible way.
I must emphasize, though, that these challenges in no way compare to the very real, difficult and often daily experience of many in this country who are just not seen, either on account of their race, class, financial status, or position in all the races we run. But, I at least caught a glimpse of Ralph Ellison’s predicament in The Invisible Man:
“When they approach me they see only my surroundings, themselves or figments of their imagination, indeed, everything and anything except me.”
In medicine, there is an irony that it is possible to look at patients very closely, yet somehow manage not to see them. We pore over chest x-rays, dissect MRIs, scrutinize pathology slides, diligently save the finest image slices of their brains in a navigation program, yet somehow miss who they are.
So how then do we see the invisible?
There is a difference between the invisibility of an object and that of a person. A truly invisible object has some intrinsic quality that makes its presence unapparent. But an invisible person is not intrinsically invisible. That invisibility is conferred. That is what is so disheartening, that we as humans would ever choose to not see someone else. But perhaps, therein lies also the possibility for change. If we can confer invisibility, we can confer visibility. Each day can be an exercise in noticing the “middle runners.” Who is invisible to you? Who can you choose to see?